MARY E. POWELL and JENNIFER TRUONG, May 2016 —
The Equal Employment Opportunity Commission (“EEOC”) issued final wellness plan rules under Title I of the Americans with Disabilities Act (“ADA”) and Title II of the Genetic Information Nondiscrimination Act (“GINA”) on May 16, 2016. The ADA rule focuses on wellness plan incentives for an employee who provides certain information about himself/herself while the GINA rule focuses on wellness plan inducements for an employee when his/her spouse discloses certain information.
Remember, these are only two of the rules that an employer must consider when it implements a wellness program. An employer must also comply with the Employee Retirement Income Security Act (“ERISA”), the Internal Revenue Code (“Code”), the Patient Protection and Affordable Care Act (“ACA”), the Health Insurance Portability and Accountability Act (“HIPAA”), federal employment laws such as the Equal Pay Act, and certain State laws, and their respective implementing regulations and other guidance. Needless to say, wellness programs are highly regulated!
ADA and Wellness Plans
The essence of this final rule is that employers may provide limited incentives (financial or in-kind) in exchange for an employee’s participation in a wellness program that includes disability-related inquiries or medical examinations. The main changes from the proposed rule to this final rule are the limitations on incentives and the notice requirement.
Background
Title I of the ADA prohibits employers from discriminating against individuals on the basis of disability. Generally, employers cannot obtain medical information from employees; however, employers are allowed to make inquiries about employees’ health or require medical examinations as part of a voluntary employee health program, which includes wellness programs.
NOTE, the rule applies to ALL wellness programs that include disability-related inquiries and/or medical examination — it does not matter if that wellness program is offered as part of, or outside of, a group health plan.
Requirement #1 — Employee Health Program That Is Reasonably Designed
A wellness program, which could include a health risk assessment, biometric screening or other similar component, must be reasonably designed to promote health or prevent disease. A program satisfies this requirement if it: (i) has a reasonable chance of improving the health of, or preventing disease in, participants; (ii) is not overly burdensome; (iii) is not a subterfuge for violating the ADA or any laws prohibiting employment discrimination; and (iv) is not highly suspect in the method chosen to promote health or prevent disease. A program that consists of a measurement, test, screening, or collection of health-related information without providing results, follow-up information, or advice designed to improve the health of participating employees is not reasonably designed, unless the collected information actually is used to design a program that addresses at least a subset of the conditions identified. Furthermore, a program is not reasonably designed if it exists mainly to shift costs to certain employees based on their health or simply to provide an employer information to estimate future health costs. Whether a program is reasonably designed is evaluated in light of all the relevant facts and circumstances. The interpretive guidance to the rule also gives examples of programs that would or would not meet this standard.
Comment: An employer cannot have a wellness program that is used solely to gain information about the health of its workforce. The wellness program cannot be overly burdensome, such as programs that require a large amount of time for participation, involve intrusive procedures, or place significant costs for medical examinations on employees.
Requirement #2 — Voluntary
The wellness program must be voluntary, which means that the employer:
(i) does not require employees to participate,
(ii) does not deny coverage under any of its group health plans or particular benefit packages within a group health plan for non-participation,
(iii) does not take any adverse employment action against employees for non-participation, or retaliate against, interfere with, coerce, intimidate, or threaten employees in violation of Section 503 of the ADA, and
(iv) provides a notice that: (A) is written so that the employee is reasonably likely to understand it, (B) describes the type of medical information that will be obtained and the purpose for which it will be used, and (C) describes the restrictions on the disclosure of the medical information, the employer representatives and other parties with whom the information will be shared, and how the employer will ensure that the information is not improperly disclosed (including whether the program complies with the privacy and security provisions under HIPAA).
Comment: The EEOC commented that some employers have begun offering health plan benefits and cost-sharing structures that base eligibility for a particular health plan (or benefit) on completing a health risk assessment or undergoing biometric screenings. The EEOC refers to these as “gateway plans.” While the rule does allow for certain incentives (described below), the ADA continues to prohibit the outright denial of access to a benefit or health plan. Therefore, these gateway plans cannot be considered voluntary.
Comment: Employers will need to revise current wellness program notices. It is unlikely that an employer’s current notice would include all of the required information. The EEOC stated it will provide an example of a notice that complies with the rule.
Requirement #3 — Incentives
The maximum allowable incentives are set forth in the chart below. The total cost takes into account both the amount the employer pays for premiums and the amount the employee pays for premiums.
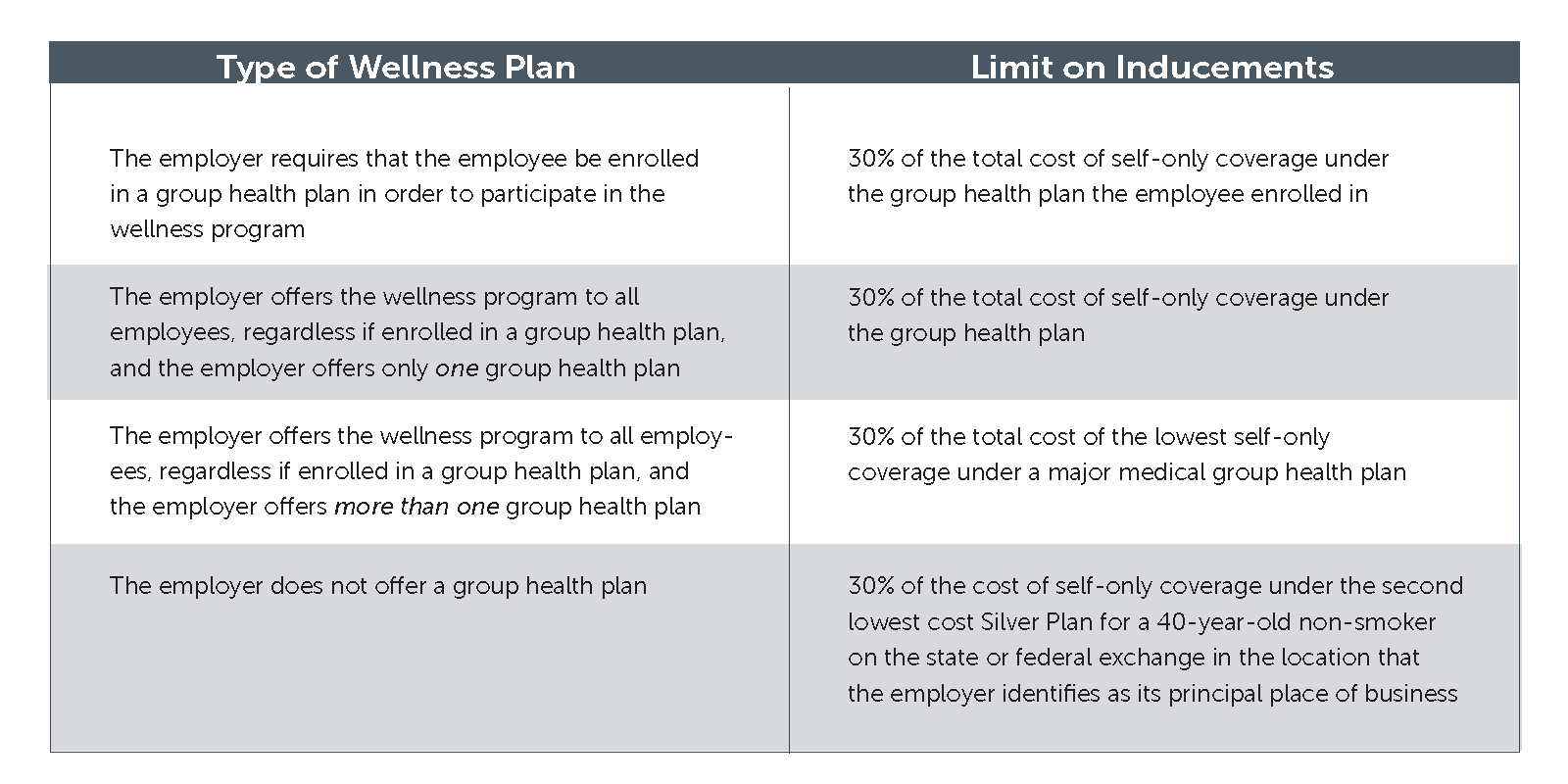
Example: An employee participates in a wellness program that is only offered to employees enrolled in a group health plan, and the total cost of self-only coverage under the group health plan is $6,000 annually (taking into account the amounts that both the employee and the employer pay for the premium). The maximum allowable incentive for the year is $1,800.
Comment: This rule discusses wellness programs that are offered to all employees — even those not enrolled in an employer’s group health plan. If the wellness program is not integrated with the group health plan, the employer will need to determine if that wellness program either complies with ACA (such as covering preventive care at no cost) or is exempt from ACA.
Comment: Not all wellness programs are subject to these ADA incentive rules. For example, the incentive rules do not apply to a wellness program that requires employees to attend nutrition classes because the program does not involve disability-related inquiries or medical examinations. However, other ADA rules may apply, such as providing a sign language interpreter so that a deaf employee could attend that nutrition class.
Comment: This incentive limit is one of the ways the ADA rule differs from HIPAA wellness program provisions. While the HIPAA provisions do not impose any incentive limits on “participatory” wellness programs, the ADA incentive limit applies to all wellness programs involving disability-related inquiries or medical examination without regard to whether the program is a participatory or health-contingent program.
Requirement #4 — Confidentiality
Any medical information must be treated as a confidential medical record, and it must be collected and maintained on separate forms and in separate medical files (different from personnel files). The employer may only receive information collected as part of the wellness program in aggregate terms that do not disclose, and are not likely to disclose, the identity of the individuals, except as necessary to administer the wellness program. Furthermore, the employer may not require an employee to agree to the sale, exchange, sharing, transfer, or other disclosure of medical information (except to carry out specific activities related to the wellness program), or waive confidentiality protections available under the ADA as a condition for participating in the wellness program or obtaining an incentive.
Comment: While this EEOC rule contains a confidentiality provision, an employer must also consider the application of the privacy and security rules under HIPAA.
Requirement #5 — Compliance with Other Employment Nondiscrimination Laws
Compliance with this rule does not mean that the wellness program will be deemed to comply with other employment nondiscrimination laws, such as Title VII of the Civil Rights Act, the Age Discrimination in Employment Act, the Equal Pay Act, etc.
Requirement #6 — Inapplicability of the ADA’s Safe Harbor Provision
The safe harbor provision referenced in the final wellness program rule states that an insurer or entity that administers benefit plans is not prohibited from establishing or administering the terms of a bona fide benefit plan based on underwriting risks. Some employers have relied on this safe harbor provision to permit large incentives or to permit practices such as requiring employees to participate in a wellness program in order to maintain coverage under a health plan. The EEOC rejected this use of the safe harbor — the final ADA rule now states that the safe harbor does not apply to wellness programs, even if the program is offered as part of the employer’s health plan. In addition, the EEOC specifically states in the preamble to the rule that it disagrees with the two court cases that relied on this safe harbor provision, Seff v. Broward County and EEOC v. Flambeau, Inc.
Comment: The EEOC is very clear that this safe harbor cannot be relied on by employers for their wellness programs. According to the EEOC, this provision does not apply to employers because employers are not collecting or using information to determine whether employees with certain health conditions are insurable (i.e., risk classification).
Smoking Cessation
If a wellness program simply asks if an employee smokes, then this ADA rule does not apply because the program does not ask a disability-related question. However, if the wellness program tests employees for nicotine use, then this ADA rule would apply because the wellness program involves a medical examination.
Applicable Date
The EEOC states that the provisions of the rule concerning notice and incentives will only apply prospectively to employer wellness programs as of the first day of the first plan year that begins on or after January 1, 2017, for the health plan used to determine the level of incentive permitted under the rule. However, the EEOC states that all other provisions of this final rule are applicable immediately because it believes that it simply clarifies existing obligations.
GINA and Wellness Programs
The essence of this final rule is that employers may provide limited inducements (financial or in-kind) in exchange for an employee’s spouse providing information about his/her manifestation of a disease or disorder as part of a wellness program. The main change from the proposed rule to this final rule is the limitations on inducements that may be offered.
Background
Title II of GINA was enacted to protect employees from employment discrimination based on their genetic information. It restricts employers from requesting, requiring or purchasing genetic information, except in a few limited circumstances. The rule applies to genetic information such as information about the genetic tests of a family member and information about the manifestation of a disease or disorder in a family member of an individual (i.e., family medical history). Family members of an individual include someone who is a dependent of an individual through marriage, birth, adoption or placement for adoption, and any other individual who is a first-, second-, third-, or fourth-degree relative. This definition of family member includes an employee’s spouse, parents and children. Although asking an employee’s spouse to disclose information about the spouse’s manifestation of disease or disorder is generally prohibited as a request for genetic information about the employee, an employer may ask about family medical history under the exception for services offered as part of a voluntary wellness program, as long as the following requirements are met.
Requirement #1 — Reasonably Designed
The wellness program must be reasonably designed to promote health or prevent disease. Generally, the wellness program meets this standard if it: (i) has a reasonable chance of improving the health of, or preventing disease in, participating individuals, (ii) is not overly burdensome, (iii) is not a subterfuge for violating Title II of GINA or other laws prohibiting employment discrimination, and (iv) is not highly suspect in the method chosen to promote health or prevent disease. Additionally, a design is unreasonable if it penalizes an employee because his/her spouse’s manifestation of disease or disorder prevents the spouse from achieving a certain health outcome for example, denying an inducement because the employee’s spouse has a blood pressure, a cholesterol level, or blood glucose level that the employer considers too high). The rule contains numerous examples of wellness programs that are not reasonably designed to promote health or prevent disease, such as a program consisting of a measurement or test of health-related information that fails to provide the individual with his results.
Comment: This requirement is very similar to the one set forth in the ADA rule above.
Requirement #2 — Genetic Information
The employer may not offer an inducement for individuals to provide genetic information (except as provided in requirement #3), but may offer inducements for the completion of a health risk assessment that includes questions about family medical history or other genetic information, so long as it is clear that the inducement will be made available regardless of whether the participant answers questions concerning genetic information.
Comment: The rule does allow an employee to receive an inducement when the spouse provides his/her information about his/her manifestation of disease or disorder. However, inducements for the disclosure of other genetic information is not permissible.
Requirement #3 — Spouse’s Manifestation of Disease or Disorder
An employer may offer an inducement to an employee whose spouse provides information about his/her manifestation of disease or disorder as part of a health risk assessment. The health risk assessment must be administered in connection with the spouse’s receipt of health or genetic services offered by the employer (e.g., an employer-sponsored wellness program). No inducement can be offered in return for: (i) the spouse providing his/her own genetic information, (ii) information about the manifestation of disease or disorder of the employee’s children, or (iii) genetic information about the employee’s children.
Comment: Essentially, no health information can be provided about an employee’s biological or adopted child, no matter the age of the child.
Requirement #4 — Authorization
The spouse must provide prior, knowing, voluntary, and written authorization when the spouse completes a health risk assessment (which may include a medical questionnaire and/or medical examination). That authorization must describe the confidentiality protections of the rule and the restrictions on disclosure of genetic information.
Comment: In the preamble to the rule, the EEOC states that although the GINA rule does not add new confidentiality requirements, Title II of GINA and existing regulations already include specific confidentiality provisions. For example, the exception that permits employers to acquire genetic information as part of a wellness program requires a signed authorization that explains: (i) the restrictions on the disclosure of that information, (ii) that individually identifiable genetic information is provided only to the individual receiving the services and the licensed health care professionals or board certified genetic counselors, and (iii) that any individually identifiable genetic information is only available for purposes of the health or genetic services and is not disclosed to the employer, except in aggregate terms.
Requirement #5 — Inducement
The limitation on inducements is similar to the ADA rule. However, the GINA rule allows the spouse and the employee to each receive the 30% inducement.
Example: The employer offers one group health plan and self-only coverage under that plan costs $7,000 (taking into account the amount that both the employee and the employer pays for the premiums). The employer provides the option of participation in a wellness program to the employee and the spouse, but they are not required to enroll in the group health plan. The employer may offer an inducement of no more than $2,100 to the employee and $2,100 to the spouse.
Comment: Like the ADA rule, this GINA rule discusses wellness programs that are offered to all employees — even those not enrolled in an employer’s group health plan. If the wellness program is not integrated with the group health plan, the employer will need to determine if that wellness program either complies with ACA (such as covering preventive care at no cost) or is exempt from ACA.
Requirement #6 — Cannot Require an Agreement to Sell and Confidentiality
An employer cannot condition participation in a wellness program on, or provide inducements in exchange for, an agreement permitting the sale, exchange, sharing, transfer or other disclosure of genetic information. Genetic information gathered as part of a wellness program can only be disclosed to the employer in aggregate terms that do not disclose the identity of specific individuals.
Requirement #7 — Cannot Deny Access
The employer may not deny access to the health plan or any package of health benefits to an employee, or the spouse or other covered dependent, or retaliate against an employee due to the spouse’s refusal to provide information about his/her manifestation of disease or disorder.
Requirement #8 — Compliance with Other Laws
This is similar to the ADA rule.
Smoking Cessation
The EEOC states that a wellness program does not request genetic information when it asks the spouse whether he/she uses tobacco or when it requires a spouse to take a blood test to determine nicotine levels. This is not information about the spouse’s manifestation of disease or disorder (i.e., genetic information) and hence this GINA rule does not apply.
Applicable Date
The EEOC states that the provisions of the rule concerning inducements will only apply prospectively to employer wellness programs as of the first day of the first plan year that begins on or after January 1, 2017, for the health plan used to determine the level of inducement permitted under the rule. However, the EEOC states that all other provisions of this final rule are applicable immediately because it believes that it simply clarifies existing obligations.



